We studied how to reduce airborne COVID spread in hospitals. Here's what we learnt
- Written by Kirsty Buising, Professor, The Peter Doherty Institute for Infection and Immunity
Melbourne’s second wave of COVID-19 last year, which led to a lockdown lasting more than 100 days, provided us with many lessons about controlling transmission. Some of these are pertinent as New South Wales endures its ongoing lockdown.
One feature of Melbourne’s second wave was a disproportionate impact on health-care workers, patients in hospital, and residents in aged-care homes. In response to this, a team of Melbourne-based infectious clinicians, engineers and aerosol scientists came together to learn from each other about how to mitigate the risk of airborne COVID-19 transmission in health care.
We are some members of that team. As we hear about COVID spreading in Sydney hospitals during the current outbreak, we want to share what we learnt about how to potentially minimise airborne COVID-19 spread in the hope it’s helpful to our colleagues.
Importantly, much has improved over the course of the pandemic. Most health-care staff and some of our patients (even if not as many as we would like) are vaccinated against COVID-19, reducing the likelihood of severe illness and death. Appropriate personal protective equipment (PPE) is generally available, including fit-tested N95 masks, and practices such as physical distancing and use of tele-health have been widely adopted.
But aerosol transmission of COVID-19 remains a very real and ongoing problem.
Read more: Australia must get serious about airborne infection transmission. Here's what we need to do
We’ve read recent expert commentaries about dealing with COVID-19 that mention paying attention to indoor ventilation. But rarely do these specify what exactly can and should be done in our existing hospital buildings.
The heating, ventilation and air conditioning systems in hospitals, like most public indoor spaces, are built for comfort and energy efficiency, not for infection control (aside from purpose-built isolation areas).
Clearly, we cannot rebuild all our hospital ventilation systems to cope with the current outbreak.
However, there are tangible things that can be done now and in future.
Our recommendations
We recommend hospitals prioritise the use of negative pressure rooms for COVID-19 infected patients where available. Negative pressure rooms are built specifically for patients with highly infectious diseases. We already use them when caring for hospitalised people with tuberculosis, measles and chickenpox.
These rooms usually have an “anteroom” with a door either side before the patient room. The air pressure is lower in the anteroom than the corridor, and then lower again in the patient room compared to the anteroom. This means potentially contaminated air doesn’t escape outside the patient room when the door is opened.
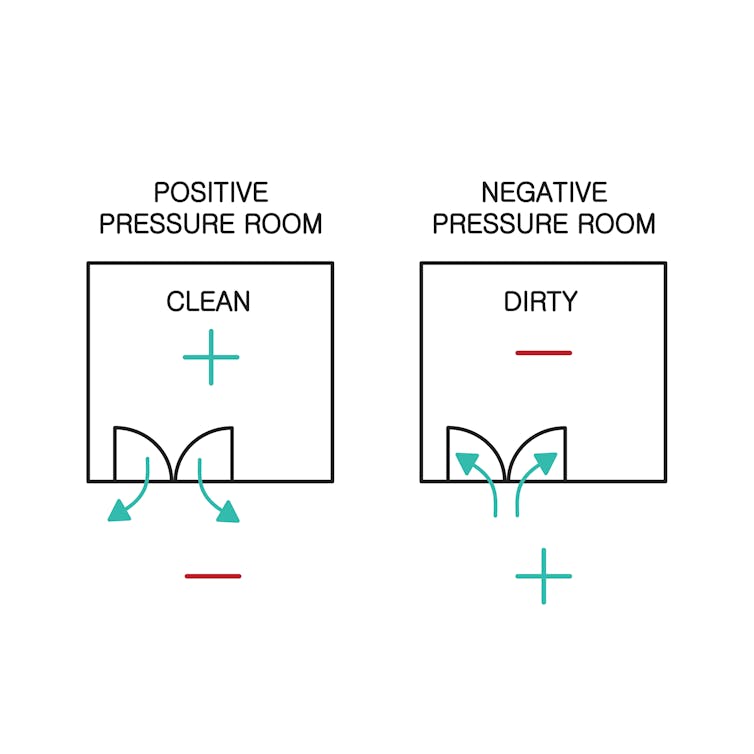 Negative pressure rooms ensure potentially contaminated air doesn’t escape into the corridor.
Shutterstock
Negative pressure rooms ensure potentially contaminated air doesn’t escape into the corridor.
Shutterstock
However, these rooms are usually in short supply even in larger hospitals, and may not exist in smaller or rural hospitals.
If negative pressure rooms aren’t available, then where possible, COVID-19 patients should be managed in single rooms with doors that close.
Preferably, these should be rooms with a high number of “air exchanges per hour”. This is a measure of the refreshing of air in the room. Six air exchanges per hour has been suggested at a minimum for hospital rooms, but preferably more.
Hospitals need to be aware the air in normal rooms can travel outside into corridors. Some rooms may be positively pressured without being labelled as such, so we recommend having them tested.
Two small air cleaners can clear 99% of infectious aerosols
If patients with COVID-19 are being managed outside negative pressure rooms, then we recommend hospitals consider using portable air cleaners with HEPA filters.
We published a world-first study in June into airflow and the movement of aerosols in a COVID-19 ward, giving us a real insight into how the virus might be transmitted.
We found portable air cleaners are highly effective in increasing the clearance of particles from the air in clinical spaces and reducing their spread to other areas.
Two small domestic air cleaners in a single patient room of a hospital ward could clear 99% of potentially infectious aerosols within 5.5 minutes.
These air cleaners are relatively cheap and commercially available. We believe they could help reduce the risk of health-care workers and other patients acquiring COVID-19 in health care.
We are currently using them at the Royal Melbourne Hospital and Western Health.
Read more: Poor ventilation may be adding to nursing homes' COVID-19 risks
Innovations such as personal ventilation hoods can also be extremely useful. Western Health’s intensive care unit, which managed large numbers of patients in Melbourne in 2020, used these hoods to filter air close to COVID-19 positive patients and help protect staff.
It’s also important hospitals perform ventilation assessments of wards to be aware of the pathways of airflow through spaces to help inform where to position patients and staff.
We found minimising the number of infected patients in a given physical space was important as we think this helped to reduce the density of aerosols. When patient numbers are high, hospitals should try to avoid caring for more than one COVID-19 positive patient in a room, if possible, which may mean closing beds.
Clearly, if new COVID-19 case numbers climb, this becomes difficult, and enlisting the help of additional hospitals with suitable facilities to “share the load” will be necessary.
New hospitals must focus on ventilation
We need to focus on practical strategies we can implement right now to retro-fit health-care settings to improve safety for staff and patients.
But we must also plan for the future.
In designing new hospitals, it’s critical to:
keep ventilation front of mind
build enough negative pressure rooms and single patient rooms
add air cleaning and air monitoring to the building operations toolbox.
We will achieve this by designing facilities together with staff.
Vaccinations will help control this current pandemic. But we’ve learnt so much about managing this virus in such a short time. Let’s apply what we’ve learnt about aerosol transmission to make practical changes to improve safety now and into the future.
The authors would like to thank Ashley Stevens, hospital engineer at Royal Melbourne Hospital, for contributing to this article and the research.
Authors: Kirsty Buising, Professor, The Peter Doherty Institute for Infection and Immunity





