We should be cautious, but not concerned: there's little evidence PFAS exposure harms our health
- Written by Ian Musgrave, Senior lecturer in Pharmacology, University of Adelaide
Per- and poly-fluorinated alkyl substances (PFAS) are persistent organic pollutants found most commonly in firefighting foam.
Every now and again, concerns around the possible health effects of exposure to PFAS pop up in the news. These chemicals don’t readily break down, and can accumulate in the environment.
PFAS contamination of water and fish was recently reported in Mackay and Darwin Harbour. Even my local free weekly paper in Adelaide had “PFAS food fright” plastered across the front page not long ago, arising from groundwater contamination near the local fire station.
Yes, PFAS might have been picked up in a few new places. But the latest evidence suggests the levels at which we’re exposed are very unlikely to affect our health.
Read more: The chemicals in firefighting foam aren't the new asbestos
What are PFAS?
PFAS (also known as perfluoroalkyl acids, or PFAAs) are long chains of carbon atoms studded with fluorine molecules. They include compounds such as perfluorooctanesulfonic acid (PFOA) and perfluorooctane sulfonate (PFOS).
PFAS are inert, water repellent and heat resistant. This makes them ideal for applications ranging from stain-resistant fabrics, to non-stick cookware, to firefighting foams.
Their chemical properties mean they’re very resistant to breakdown and persist in the environment for many years. Even though these PFAS started to be phased out in 2000, they still linger in some places where firefighting foams were used extensively, such as fire stations and airports.
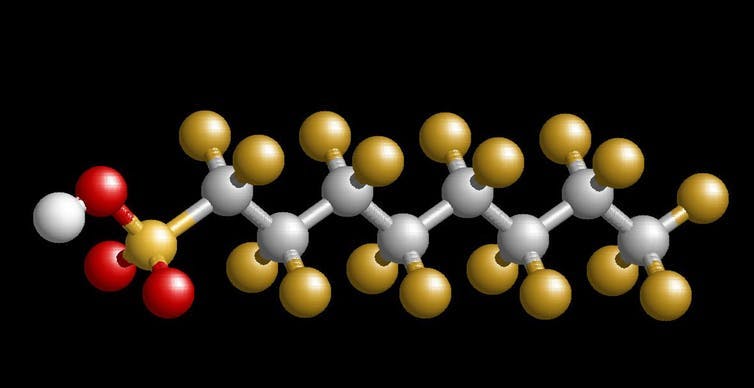 The chemical structure of perfluorooctanesulfonic acid (PFOA), a typical PFAS.
Ian Musgrave
The chemical structure of perfluorooctanesulfonic acid (PFOA), a typical PFAS.
Ian Musgrave
Where do PFAS come from?
In an Australian context, the most important sources of PFAS originate in their use for firefighting. The firefighting foam enters the soil around the site where a fire has occurred, or gets into storm-water drains. From there, it ends up in either the groundwater or streams, and ultimately the ocean.
Drinking water is not a major source of PFAS in Australia, as we typically don’t use groundwater for drinking. But in some places, groundwater contaminated with PFAS is used to irrigate food plants, and can enter the food chain through plants retaining PFAS from the water. This is the basis of the headline in my local paper, as many local residents use bore water for their fruit and vegetable gardens.
Read more: Companies should take charge of the potential toxins in common products
In a food chain, small amounts of PFAS can be concentrated as you move up the chain from plants to insects to fish. That is, insects may feed on affected plants, and fish may eat affected insects. So fish in rivers or bays contaminated with PFAS runoff can be a substantial source of PFAS. This is the issue in Mackay and Darwin.
Notably, the exposure people might face from eating affected fish or crops is below the levels people exposed to PFAS in an industrial sense, like firefighters, would encounter.
PFAS and health: the experts respond
PFAS take a long time to break down in organisms. For example, in humans, it takes around five years for half an ingested dose of PFOA to pass through the system.
The build-up of a chemical that’s hard to remove from our bodies is always of concern. I wrote in an earlier article in 2017 that despite this, the potential health risks appeared to be low.
Since then, the Australian Expert Health Panel for PFAS looked in detail at the evidence, publishing its findings last year.
If anything, there appears to be even less risk from PFAS than we thought.
How do we study these potential health effects?
We can do studies on animals; these are indicative but can be misleading. For example, the effects of PFAS on what’s called peroxisome proliferation receptors that regulate fats have been measured in rodents.
The effects occur at concentrations typically 1,000 times higher than average human blood concentrations, and around 100 times the blood concentrations in contaminated workers. The human system is less sensitive than the mouse system, so mouse and rat studies may overestimate toxicity to humans.
We can do longitudinal studies where we follow PFAS exposure and health outcomes in humans over time. But a lack of good exposure monitoring and the difficulty in accounting for other environmental influences makes it hard to reach clear conclusions.
Studies of industrial workers exposed to high environmental levels of PFAS give an idea of what exposure to high levels can do, but are less helpful for low levels.
But synthesising all this data, as done by the expert panel, helps overcome these limitations.
Read more: How microplastics make their way up the ocean food chain into fish
The most pressing concern on people’s minds is cancer, but there’s no consistent evidence PFAS is associated with cancer. One study even found exposure to PFOA decreased the incidence of bowel cancer.
The expert health panel report concluded “there is no current evidence that suggests an increase in overall cancer risk”.
The other major concern is heart disease risk. But studies of people who have been chronically exposed to significant levels of PFOA have not shown statistically significant increases in heart disease.
Similarly, no consistent findings have linked PFAS to any other health concerns previously expressed, which have included reduced kidney function, altered immune response, and earlier menopause.
 In Australia, the most common source of PFAS is firefighting foam.
From shutterstock.com
In Australia, the most common source of PFAS is firefighting foam.
From shutterstock.com
What’s the take home message?
The panel concluded there is mostly limited or no evidence for PFAS having any link with human disease.
Though they noted even though the evidence for PFAS exposure and links to health effects is very weak and inconsistent, health effects for people exposed to PFAS cannot be ruled out based on the current evidence.
But the take home message is don’t panic. Most people will be getting less than the tolerable daily intake of these chemicals from their food and water (that is, below a threshold that would cause any potential adverse health effects).
To err on the side of caution, it’s sensible to minimise exposure by not consuming fish from affected areas or limiting bore water use for irrigating suburban gardens near contamination sites.
Read more: Is your health at risk from fish and frying pans?
Authors: Ian Musgrave, Senior lecturer in Pharmacology, University of Adelaide





