Hospital beds and coronavirus test centres are needed fast. Here's an Australian-designed solution
- Written by Deborah Ascher Barnstone, Professor, Course Director Undergraduate Studies, School of Architecture, University of Technology Sydney
Two of the most pressing needs worldwide in the coronavirus pandemic are for more hospital beds and testing centres. No country in the world has enough hospital beds or intensive-care unit (ICU) beds for a pandemic. Even the best prepared, like Germany with 33.9 ICU beds per 100,000 citizens, does not have enough.
Most countries have locked down to buy time by flattening the infection curve so fewer patients will present to hospital at once. They hope to use the time to boost hospital capacity.
Read more: What steps hospitals can take if coronavirus leads to a shortage of beds
But the design challenge is significant. We need structures that can be quickly and easily assembled, are inexpensive and meet technical requirements. Architects have always worked on such challenges – the Living Shelter is one recent example.
Here in Australia a consortium is working to develop two designs, one for hospital intensive care units and one for COVID-19 testing centres, that can be used across the country and overseas. By using recycled shipping containers as the core structure, the price of the buildings will be less than a third of the cost of conventional designs.
In both building types, the container doubles as structure and packaging. This means the designs are self-contained and easy to distribute anywhere in the world. All the building parts, technical equipment, cabinets and other fit-out materials pack into the container.
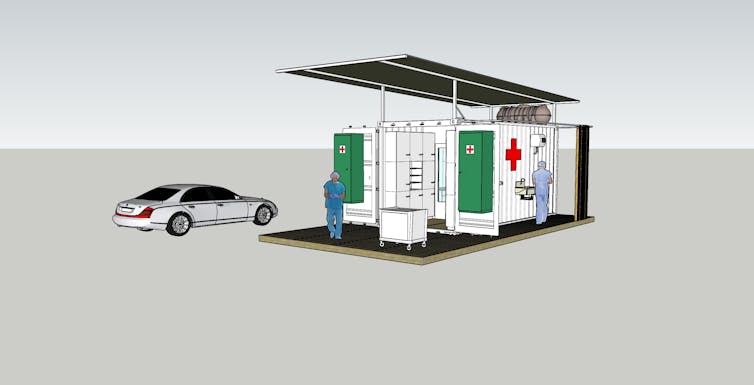
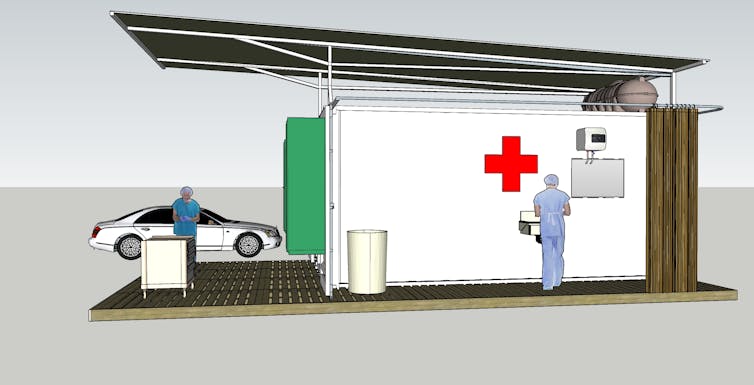 The design of the testing centre is based on a shipping container, which doubles as the packaging for transport.
Author provided
The design of the testing centre is based on a shipping container, which doubles as the packaging for transport.
Author provided
Douglas Abdiel, the director of charitable foundation P&G Purpose, and architect Robert Barnstone are working together on the design and delivery of these hospital units and testing centres.
Barnstone specialises in disaster relief architecture. He has developed designs for emergency housing for the International Red Cross and rapid deployment schools for countries afflicted by disaster. This experience gave Barnstone invaluable insights into the economics and potential construction systems for the hospital units and testing centres.
Read more: Coronavirus will devastate Aboriginal communities if we don't act now
What are the key requirements?
Any disaster relief architecture must consider several critical design aspects:
buildings need to be as cheap as possible so limited funds can be stretched to help as many people as possible
the structure should be lightweight and easy to assemble because professional builders might not be available for construction
the structure needs to be weatherproof and insulated for variable climates
medical functions require running water, electricity, air exchange to bring fresh air into the container, and air conditioning to control the temperature inside.
The mechanical services needed in a medical facility are highly specialised and expensive. This makes it particularly challenging to design. Ideally, the structure should be lasting, so money invested in relief efforts is not wasted.
Emergency structures should also be designed for easy packaging and shipping. Standard dimensions of shipping containers, freight costs and delivery logistics must be considered.
Read more: Coronavirus an ‘existential threat’ to Africa and her crowded slums
So how do the two building designs work?
The two proposals for intensive care units and testing facilities use modified shipping containers as the supporting structure. You can see the full designs and specifications here.
The hospital structure is simply a large shed that houses ICU bays. A nurses’ station is located in the centre.
The testing centre is a drive-by place to conduct COVID-19 tests and either process them when a fast test is available or store them for shipping to laboratories.
Used shipping containers are cheap and easy to find. They are made from a steel frame with corrugated steel panelling, which makes them very strong.
Both schemes use prefabricated panels for exterior and interior walls. Window units will be integrated into panels. These come in standard sizes that easily pop into place.
The two design approaches do have differences, however.
 The front entry of the rapid deployment hospital annexe.
The front entry of the rapid deployment hospital annexe.
The hospital uses a full-length 12-metre container. The shipping container acts as the structural and spatial core of the hospital building.
When unpacked, the container sits in the middle of the hospital and supports long-span steel trusses and the roof. It houses office and storage space.
 Inside the hospital annexe the container houses the nurses’ annexe and supports the building trusses and roof.
Inside the hospital annexe the container houses the nurses’ annexe and supports the building trusses and roof.
The prefabricated panels form both the outside walls and interior partitions. End walls are made of transparent glass to allow natural light into the interior.
Interior bays for patients are also prefabricated. These line the exterior walls, leaving space for hospital staff to circulate between the ICU bays and central container.
In contrast, the testing centre is a single-unit building made from a half-length six-metre container. A large overhanging canopy covers the roof and front deck to protect against sun and rain.
A water storage tank rests on the roof underneath the canopy. A generator sits on one side. There is a scrub sink and changing area outside, with a curtain that allows for privacy and a bin to dispose of protective equipment.
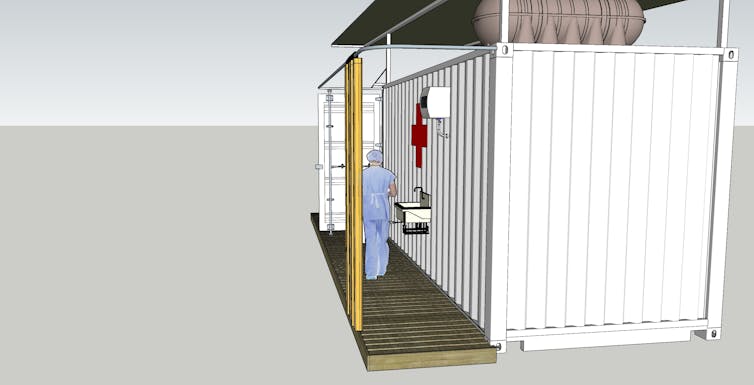 The exterior of the testing centre has a changing area and sink.
The exterior of the testing centre has a changing area and sink.
The container doors support storage cabinets for test kits on their inside wall. These doors can swing open so they are flush with the front facade. In this position, the cabinets face the front deck for easy access by nurses and doctors.
 The front deck of the testing centre showing storage cabinets.
The front deck of the testing centre showing storage cabinets.
The interior has ample storage and office furniture.
 The testing centre office.
The testing centre office.
Construction of the prototype test centre was due to begin on April 15. To date, the team has raised A$30,000 to support the effort but needs $20,000 more. At A$3,125 per square metre, compared with about A$10,000 per square metre for usual construction, these solutions are affordable and can be produced and delivered very quickly.
Authors: Deborah Ascher Barnstone, Professor, Course Director Undergraduate Studies, School of Architecture, University of Technology Sydney




