Want to improve care in nursing homes? Mandate minimum staffing levels
- Written by Julie Henderson, Research Associate, Southgate Institute for Health, Society and Equity, Flinders University
The Royal Commission into aged care has begun its 18-month investigation into the quality and safety of Australia’s residential aged-care system.
Topping the list of priorities is to uncover substandard care, mistreatment and abuse, and to identify the system failures and actions that should be taken in response.
But we don’t need a royal commission to tell us the number-one thing that can improve care in nursing homes: implementing minimum staffing levels.
Read more: Essential reading to get your head around Australia's aged care crisis
Based on our research from 2016, the Australian Nursing and Midwifery Federation recommends residents receive 4 hours and 18 minutes of care per day for optimal health and well-being.
It’s also important to get the right mix of staff performing for these hours and minutes. Half of the care should be provided by care workers (who undertake a short TAFE course), 30% by registered nurses (who complete a three-year bachelor degree at university), and 20% by enrolled nurses (who complete an 18-month diploma).
Nurse ratios in hospitals
It’s no surprise nurse shortages affect patient care. Nurse staffing shortfalls in hospitals have been associated with poorer patient outcomes, longer stays in hospital, and a higher risk of death within 30 days of discharge.
Poor staffing causes stress and frustration among nurses, who constantly feel rushed and unable to provide the type of care their patients deserve. This leads to greater job dissatisfaction and burnout.
One way to ensure nurse staffing levels is to implement mandatory nurse-to-patient ratios. California did this in 1999, when it mandated ratios ranging from one nurse to two patients in intensive care, to one nurse to six patients for women who had given birth.
Read more: Australia's aged care residents are very sick, yet the government doesn't prioritise medical care
After the ratios were implemented, the nurses’ patient loads decreased and they reported being able to provide better quality care. They also felt more job satisfaction and were less likely to burn out. Importantly, rates of complications and premature death decreased.
Minimum aged-care staffing
Seemingly small tasks in aged care can have a big impact on residents. If they don’t receive adequate assistance at meal times, for instance, they may lose weight and become malnourished. If they’re bed-bound and aren’t moved frequently enough, they’re at risk of developing painful pressure sores.
As with hospital-based care, minimum staffing ensures staff have enough time to complete these important tasks and has been associated with improvements in health outcomes for residents with multiple illnesses.
 Missed or delayed care can have an enormous impact on residents.
Elien Dumon/
Missed or delayed care can have an enormous impact on residents.
Elien Dumon/
Importantly, increasing direct care hours reduces the use of medication to manage difficult resident behaviour, allowing residents to maintain their independence.
Increasing direct nursing care also decreases the likelihood of residents being transferred to emergency departments, as their symptoms can be managed in the facility.
One key downside, however, is that the introduction of minimum staffing levels can result in a shift away from employment of registered nurses towards staff with less education and skills, as has happened in the United States.
What happens in Australia?
All Australian states and territories have legislation to determine the minimum staffing levels in hospitals to ensure patients receive timely care and close monitoring. But no such legislation exists in the aged-care sector.
The current Australian Aged Care Quality Agency standards say aged-care facilities need to be adequately staffed with appropriately skilled and qualified staff but they don’t specify what constitutes adequate.
In 2015, residents in Australian aged-care facilities received 39.8 hours of direct care per fortnight. This averaged 2.86 hours per resident per day and is significantly below the recommended 4 hours 18 minutes per day.
Read more: What is 'quality' in aged care? Here's what studies (and our readers) say
Our research, commissioned by the Australian Nursing and Midwifery Federation commissioned research, set out to investigate what constitutes safe levels of staffing in residential aged care.
In phase one, we tested six “profiles” for residents requiring between 2.5 and 5 hours of nursing care daily, using the de-identified data of 200 residents. We then recruited experienced registered nurses to time and record what amounted to nearly 2,000 nursing and personal care interactions in hospitals, aged care and rehabilitation facilities.
We ran the six “profiles” made up of timed care activities through seven focus groups of nurses working in aged care to determine the proportion of residents who meet each profile.
 Nurses and carers want the time to provide quality care to residents.
Alexander Raths/Shutterstock
Nurses and carers want the time to provide quality care to residents.
Alexander Raths/Shutterstock
Overall, we found more than 60% of aged care residents required four or more hours of care per day. This rate is likely to be similar in most aged-care facilities across the country.
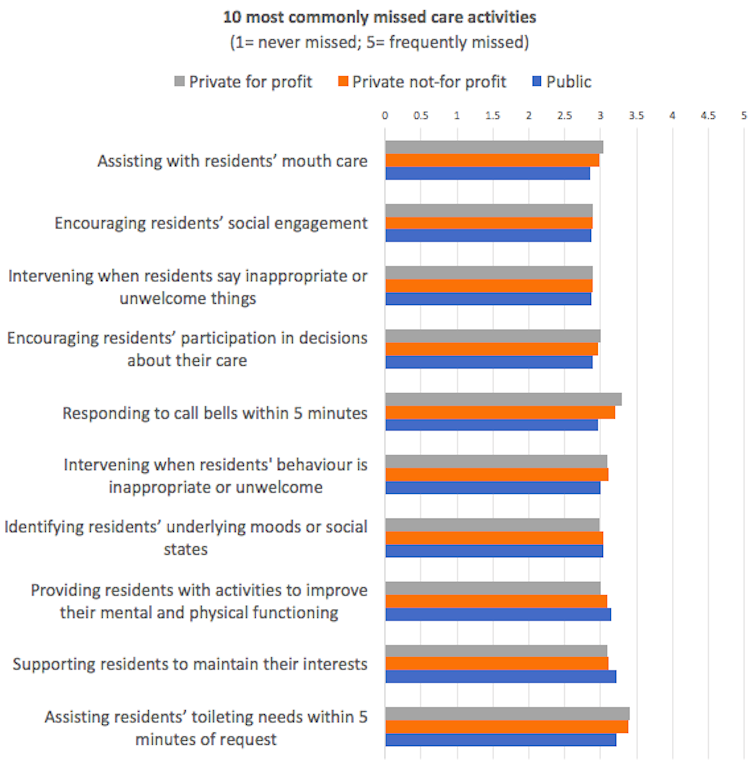
The second component of our research involved surveying 3,206 staff working in aged care to determine the amount and types of care missed and the reasons why. This is care missed or delayed because of multiple demands, inadequate staffing and material resources, or communication breakdowns.
Staff believed care was being missed in all facilities, with higher levels of missed care reported in privately owned facilities (both for-profit and not-for-profit).
 Author provided
Unscheduled tasks such as responding to call bells and to toileting needs within five minutes were most likely to be missed – as were the social and behavioural needs of residents.
Complex care activities such as wound care, medication and end-of-life care were less likely to be missed, although there were deficits in some areas.
When asked to indicate the reasons why care was missed, the respondents cited:
having too few staff
the complexity of resident needs (for example, more residents receiving palliative care and with dementia)
inadequate skill mix of nursing and care work staff
unbalanced resident allocation (some staff having heavier workloads than others).
Beware cost saving
Many of the problems in the aged-care sector can be addressed with adequate staffing, and ensuring residents receive, at a minimum, the required 4 hours and 18 minutes of care each day. But staffing hours should not be increased by replacing nursing staff (who have clinical education and skills) with lower-skilled care workers.
Read more:
Aged care failures show how little we value older people – and those who care for them
In recent years, some residential aged-care providers have been reducing the number of enrolled nurses employed and substituting them with care workers to offset staffing costs. Between 2003 and 2012, 21,000 more care workers were employed, along with 2,326 fewer registered nurses.
It’s important to ensure the skill mix includes enough registered nurses for the complex assessment and specialised nursing care now required by residents.
It’s clear the royal commission must investigate staffing shortfalls rather than simply blame nurses and carers who often struggle to provide the level of care they’d like to.
Read more:
FactCheck: is the Coalition spending '$1 billion extra, every year' on aged care?
Author provided
Unscheduled tasks such as responding to call bells and to toileting needs within five minutes were most likely to be missed – as were the social and behavioural needs of residents.
Complex care activities such as wound care, medication and end-of-life care were less likely to be missed, although there were deficits in some areas.
When asked to indicate the reasons why care was missed, the respondents cited:
having too few staff
the complexity of resident needs (for example, more residents receiving palliative care and with dementia)
inadequate skill mix of nursing and care work staff
unbalanced resident allocation (some staff having heavier workloads than others).
Beware cost saving
Many of the problems in the aged-care sector can be addressed with adequate staffing, and ensuring residents receive, at a minimum, the required 4 hours and 18 minutes of care each day. But staffing hours should not be increased by replacing nursing staff (who have clinical education and skills) with lower-skilled care workers.
Read more:
Aged care failures show how little we value older people – and those who care for them
In recent years, some residential aged-care providers have been reducing the number of enrolled nurses employed and substituting them with care workers to offset staffing costs. Between 2003 and 2012, 21,000 more care workers were employed, along with 2,326 fewer registered nurses.
It’s important to ensure the skill mix includes enough registered nurses for the complex assessment and specialised nursing care now required by residents.
It’s clear the royal commission must investigate staffing shortfalls rather than simply blame nurses and carers who often struggle to provide the level of care they’d like to.
Read more:
FactCheck: is the Coalition spending '$1 billion extra, every year' on aged care?
Authors: Julie Henderson, Research Associate, Southgate Institute for Health, Society and Equity, Flinders University





