Stroke, cancer and other chronic diseases more likely for those with poor mental health
- Written by Ben Harris, Policy Associate, Australian Health Policy Collaboration, Victoria University
Four million Australians, including our friends, family members, co-workers and neighbours, are living with mental health conditions, including anxiety and depression.
A new report out today from the Australian Health Policy Collaboration has found these four million Australians are at much greater risk of chronic physical disease and much greater risk of early death.
Having a mental health condition increases the risk of every major chronic disease. Heart disease, high blood pressure, arthritis, back pain, diabetes, asthma, bronchitis, emphysema and cancer are all much more likely to occur among people with anxiety and depression.
More than 2.4 million people have both a mental and at least one physical health condition.
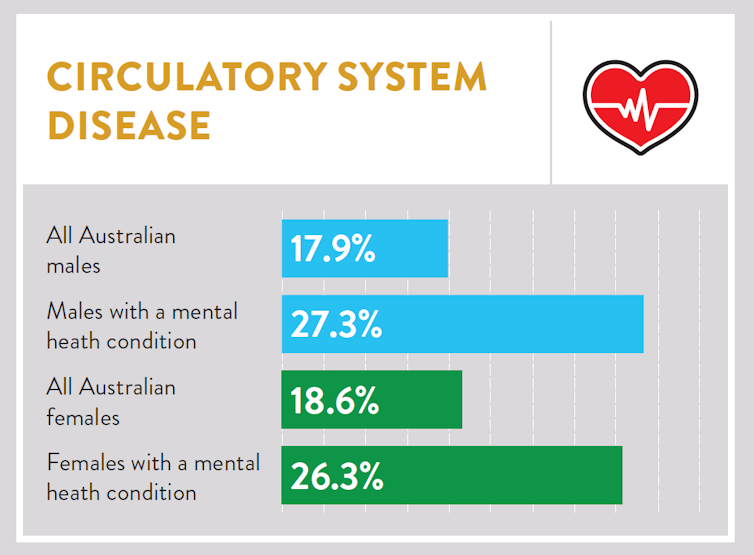
For the first time in Australia, this report quantifies the extent of this problem. For example, people with mental health conditions are more likely to have a circulatory system disease (that is, heart disease, high blood pressure and stroke). The likelihood increases by 52% for men, and 41% for women.
 Australian Health Policy Collaboration, Author provided
More than a million people are affected by both a circulatory system disease and a mental health condition. These diseases are Australia’s biggest killers.
Read more:
How Australians Die: cause #1 – heart diseases and stroke
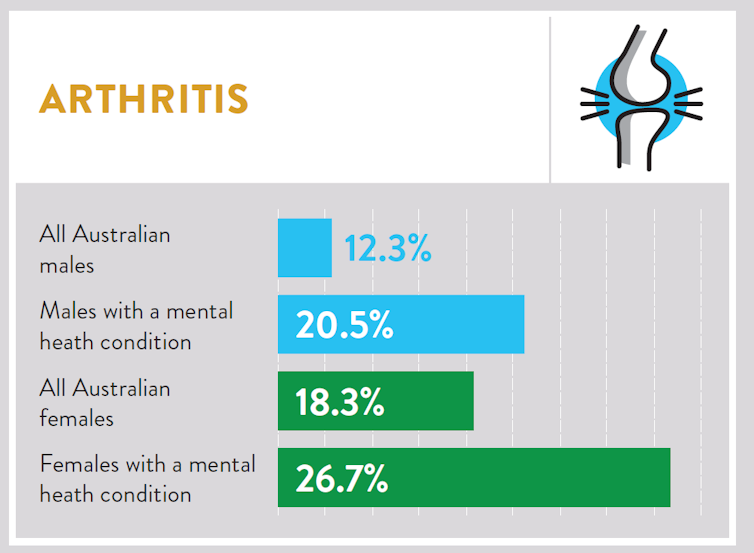
For painful, debilitating conditions such as arthritis and back pain, the numbers are even higher. Arthritis is 66% more likely for men with mental health conditions, and 46% more likely for women, with 959,000 people affected.
Australian Health Policy Collaboration, Author provided
More than a million people are affected by both a circulatory system disease and a mental health condition. These diseases are Australia’s biggest killers.
Read more:
How Australians Die: cause #1 – heart diseases and stroke
For painful, debilitating conditions such as arthritis and back pain, the numbers are even higher. Arthritis is 66% more likely for men with mental health conditions, and 46% more likely for women, with 959,000 people affected.
 Australian Health Policy Collaboration, Author provided
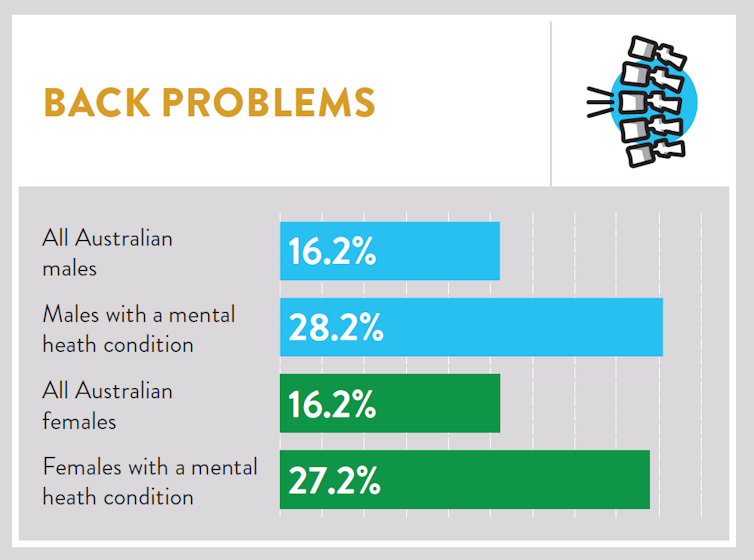
Back pain is 74% more likely for men with mental health conditions, and 68% more likely for women, with more than a million affected.
Australian Health Policy Collaboration, Author provided
Back pain is 74% more likely for men with mental health conditions, and 68% more likely for women, with more than a million affected.
 Australian Health Policy Collaboration, Author provided
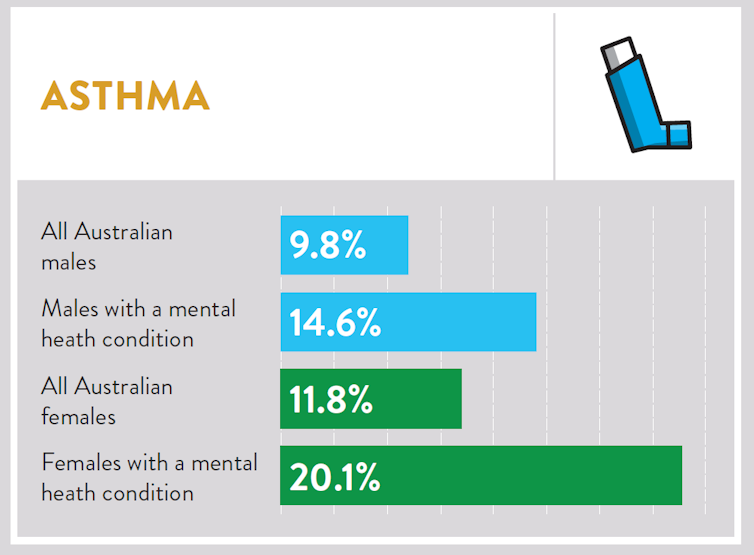
The gender differences are significant. Women with mental health conditions are much more likely to have asthma than women across Australia as a whole (70% more likely), while men are 49% more likely to have asthma with a mental health condition.
Australian Health Policy Collaboration, Author provided
The gender differences are significant. Women with mental health conditions are much more likely to have asthma than women across Australia as a whole (70% more likely), while men are 49% more likely to have asthma with a mental health condition.
 Australian Health Policy Collaboration, Author provided
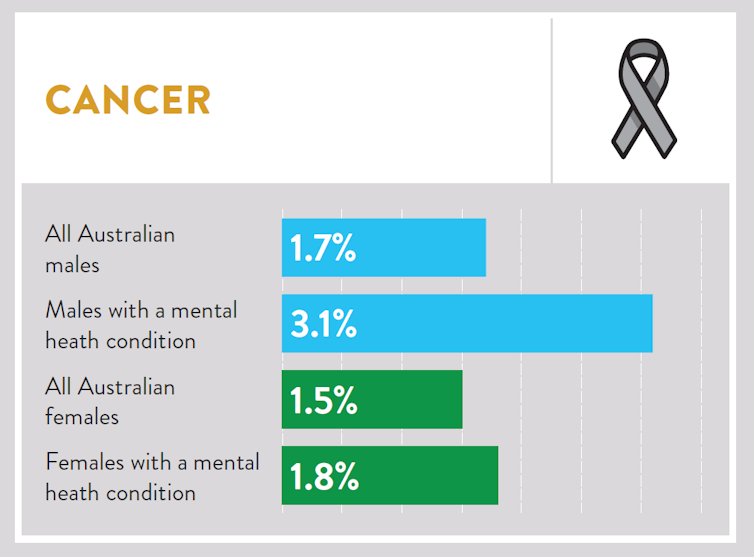
The biggest gender difference is cancer. Men with mental health conditions are 84% more likely to have cancer than the general population, and for women the figure is 20%.
Australian Health Policy Collaboration, Author provided
The biggest gender difference is cancer. Men with mental health conditions are 84% more likely to have cancer than the general population, and for women the figure is 20%.
 Australian Health Policy Collaboration, Author provided
As more women live with mental health conditions than men, overall, women are 23% more likely to be living with both a mental and physical health condition than men.
The report shows having a co-existing mental health condition and chronic physical disease generally results in worse quality of life, greater functional decline, needing to use more health care and higher healthcare costs.
These people require more treatment, use more medications, and have to spend more time, energy and money managing their health. People with a mental health condition are also more likely to be poorer, less likely to work, less likely to receive health screening and, sadly, more likely to receive substandard care for their physical diseases.
Read more:
Physical health ignored in people with mental illness
On average, people with mental health conditions die younger than the general population, and mostly from preventable conditions. We know from earlier researchthat people with severe mental illnesses die much earlier than the rest of the population. Our report shows even common mental health conditions such as anxiety and depression contribute to more chronic disease, leading to higher rates of early death.
Why?
We don’t know exactly why people with mental health conditions have poorer physical health. The Academy of Medical Sciences has identified that poor mental health and psychosocial risk factors such as feeling dissatisfied with life, not feeling calm, having sleep problems that affect work, and financial concerns can predict physical disease.
Other factors, such as low socioeconomic status, poor social networks, living in rural areas and smoking are associated with both poor mental health and poor physical health.
We do know people with mental health conditions often don’t receive advice about healthy lifestyles, don’t get common tests for disease, and are less likely to receive treatment for disease. Some of this is due to stigma and discrimination, and sometimes it’s neglect. People with mental health conditions can fall through the gaps between disjointed physical and mental health systems.
What can we do about it?
There is momentum for change among the mental health sector, with dozens of organisations signing up to the Equally Well consensus statement. This aims to improve the quality of life of people living with mental illness by providing equal access to quality health care.
There’s some great work being done around the country, including in the Hunter region, where people with mental health conditions can access tailored help with physical health risk factors such as smoking and diet.
People using mental health services should have their physical health regularly assessed, and any problems addressed as early as possible. Better coordination of care would preserve healthcare resources and improve quality of life.
Australian Health Policy Collaboration, Author provided
As more women live with mental health conditions than men, overall, women are 23% more likely to be living with both a mental and physical health condition than men.
The report shows having a co-existing mental health condition and chronic physical disease generally results in worse quality of life, greater functional decline, needing to use more health care and higher healthcare costs.
These people require more treatment, use more medications, and have to spend more time, energy and money managing their health. People with a mental health condition are also more likely to be poorer, less likely to work, less likely to receive health screening and, sadly, more likely to receive substandard care for their physical diseases.
Read more:
Physical health ignored in people with mental illness
On average, people with mental health conditions die younger than the general population, and mostly from preventable conditions. We know from earlier researchthat people with severe mental illnesses die much earlier than the rest of the population. Our report shows even common mental health conditions such as anxiety and depression contribute to more chronic disease, leading to higher rates of early death.
Why?
We don’t know exactly why people with mental health conditions have poorer physical health. The Academy of Medical Sciences has identified that poor mental health and psychosocial risk factors such as feeling dissatisfied with life, not feeling calm, having sleep problems that affect work, and financial concerns can predict physical disease.
Other factors, such as low socioeconomic status, poor social networks, living in rural areas and smoking are associated with both poor mental health and poor physical health.
We do know people with mental health conditions often don’t receive advice about healthy lifestyles, don’t get common tests for disease, and are less likely to receive treatment for disease. Some of this is due to stigma and discrimination, and sometimes it’s neglect. People with mental health conditions can fall through the gaps between disjointed physical and mental health systems.
What can we do about it?
There is momentum for change among the mental health sector, with dozens of organisations signing up to the Equally Well consensus statement. This aims to improve the quality of life of people living with mental illness by providing equal access to quality health care.
There’s some great work being done around the country, including in the Hunter region, where people with mental health conditions can access tailored help with physical health risk factors such as smoking and diet.
People using mental health services should have their physical health regularly assessed, and any problems addressed as early as possible. Better coordination of care would preserve healthcare resources and improve quality of life.
Authors: Ben Harris, Policy Associate, Australian Health Policy Collaboration, Victoria University





