Another COVID winter is coming. Is this the calm before another peak?
- Written by Catherine Bennett, Chair in Epidemiology, Deakin University
Australia is currently experiencing the longest break between infection peaks since Omicron arrived in late 2021 and community-wide transmission took off.
With winter looming, it’s worth taking stock of where we are with COVID and what we might expect over the colder months – especially in the southern states and territories. The climate and the way our behaviour changes at this time of year increase the transmission potential for all infectious respiratory diseases.
This will be our second winter with Omicron subvariants, but there are signs it might not be as challenging as the last.
Read more: Haven't had COVID or a vaccine dose in the past six months? Consider getting a booster
Peaks and troughs
The last time we had national hospital counts above 2,400 was on January 20, some 12 weeks ago. Our dips in the Omicron era have previously been short lived. Variant BA.2 replaced BA.1 quickly this time last year and hospital counts rose above 2,400 within five weeks of the first wave. In November 2022, the hospital counts again climbed above 2,400 with a change in subvariants after only ten weeks of respite.
Will the current break last? Most states are seeing a rise in hospital numbers, but those that started climbing earliest (New South Wales, Victoria and Tasmania) might already be seeing hospital numbers levelling out. So there is hope the current surge will not lead to as high rates of severe illness.
And we know, COVID counts recorded for hospitals aren’t all admissions for COVID. Most are incidental infections. Tasmanian data show on average less than one third of COVID positive patients were admitted for COVID illness.
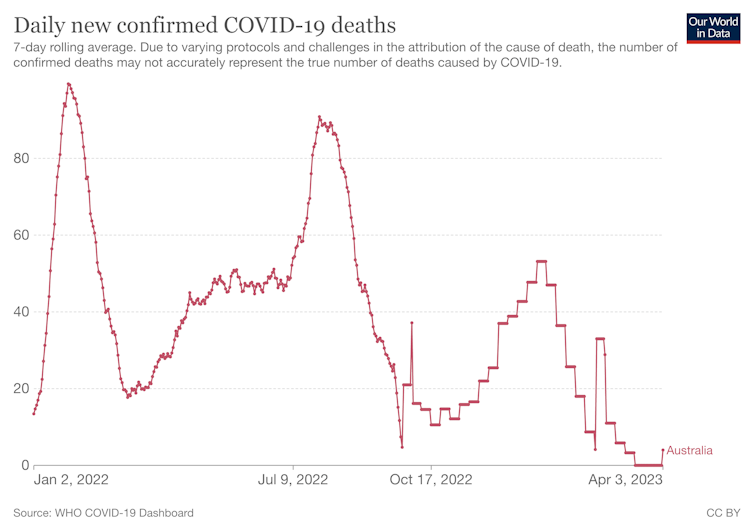
With each wave, a smaller proportion of COVID positive patients are being reported in ICU. The proportion of people on ventilators because of COVID has also reduced to less than 10% from 30% in the initial January 2022 Omicron peak. The deaths associated with each peak have also fallen with each main wave, with the summer wave just passed having about half the daily deaths reported at its peak compared with our previous summer. Antivirals have played an important role, but so too has population immunity, now estimated at 99.6%.
Community immunity
Thankfully, Omicron is less likely to cause severe illness, especially in a population with significant levels of immunity from both vaccine and prior infection. Antivirals also reduces the risk that infections will end up in hospital. But at times of peak infections, even a smaller proportion translates to significant loss of life among those who are vulnerable.
The shift in the dominant Omicron subvariants and their immune escape characteristics allow people to acquire new infections sooner than they might have if only exposed to the same variant they were infected with previously. Add to this the fact we now have a mix of variants in the population at any one time, then reinfections become more common and the overall infection rate will rise. So, while high levels of population immunity reduce the impact of infection, multiple variants circulating means infection rates can still rise.
Surveillance data from NSW show this time last year there were only two Omicron variants in circulation, BA.1. and BA.2. Now genomic testing is capturing 12 different Omicron variants and the dominant variants keep shifting, with XBB emerging as the most dominant strain alongside XBB1.5.
Getting COVID again … and again
Reinfection is difficult to measure and will be seriously underestimated due to low reporting rates and mild or asymptomatic infections.
Reinfections help fuel infection rates and therefore increase the risk of exposure to people who are at risk of severe disease if infected.
We are still not sure whether having repeat infections might alter the chances of developing long COVID. It seems less likely for Omicron, especially in people who experience mild or no symptoms.
Young adults are still the group where most infections and reinfections occur. They should be conscious of the extra risks in the winter months with more indoor mixing and make sure they’ve have had at least one booster to reduce their long COVID risk.





