Paid on par with cleaners: the broader issue affecting the quality of aged care
- Written by Ben Farr-Wharton, Associate Dean of Management, Edith Cowan University
The aged care royal commission is due to hand down its final report on February 26, and it will be tabled in parliament in the days after that.
The long-term sustainability of the aged-care workforce and the financial health of the sector more broadly, have been hot topics, regularly under the microscope as part of the royal commission.
Underpinning this focus is a belief that quality health and well-being outcomes of elderly Australians in our aged-care system is impacted by the staff who service them, and the funding arrangements of aged-care organisations themselves.
Our research into the Australian aged care sector strongly supports the need to revise existing policy, ensuring aged-care organisations are adequately staffed and resourced. When that happens, residents will receive a higher quality of care.
Pay and aged-care work
But there is a deeper problem that remains largely overlooked: the payment of aged-care workers.
 Screen Shot at am.
Author provided
Screen Shot at am.
Author provided
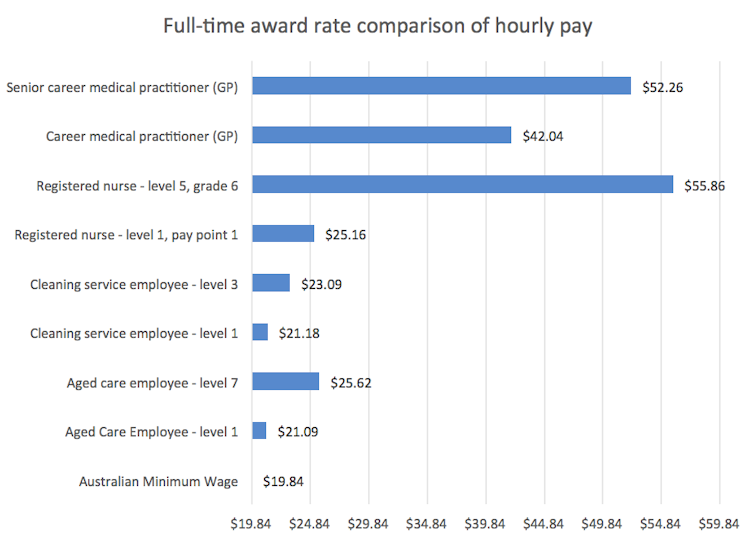
When beginning their career, the award rate for a full-time aged care worker is A$21.09 per hour - slightly less than a cleaner, and only $1.25 per hour more than the Australian minimum wage.
It goes without saying that aged-care workers do much more than clean. Although ensuring cleanliness and hygiene is certainly a component of aged-care duties, the job is substantially more complex and demanding, both physically and emotionally.
Aged-care work involves a broad spectrum of tasks: administering medication, identifying and treating pressure injuries, feeding, helping with mobility, facilitating choirs, card games and group excursions, and more.
Working in aged care requires someone who is engaged, focused, well-trained and ready to thrive in challenging clinical and social environments. Aged-care workers also need to contend with the emotional grief associated with end-of-life care and death. They need to do this while professionally engaging with families who themselves may be grief-stricken.
That we have allowed this vital work to be so poorly remunerated and under-resourced is a grim reality that our society, and our government, need to face.
Societal values have radically shifted over the past decade - with the community expecting very high levels of quality care, and there is now an appetite for change in the way we value ageing, and those who work in aged care.
So, how might we restructure aged care to more appropriately pay the workforce, and improve outcomes for the elderly?
Lessons from nursing
Parallels can be drawn between the current state of our aged-care sector and that of the nursing profession in the first half of the 20th century. At that time, nurses were widely regarded as little more than cleaners and carers who happened to work in hospitals — reflecting the snail-paced change since Florence Nightingale’s innovations during after her military nursing in the Crimean war.
Over time, however, as societal values (particularly regarding the role of women) have shifted, it has become impossible to ignore the fact that nurses play a substantial clinical role for patients.
Slowly, and as recently as the early 2000s, nursing was becoming fully professionalised. Along with this came the requirement that registered nurses have university training. Now, the role that nurses play in clinical care in hospitals is central, perhaps even more so than doctors. This is particularly because patients’ contact time with nurses is generally greater than with doctors.
 Over the past half-century nursing has slowly but surely become more professionalised.
Albert Perez/AAP Image
Over the past half-century nursing has slowly but surely become more professionalised.
Albert Perez/AAP Image
To be a nurse is to enter a profession that is highly valued, respected and relatively well-paid. The base award for a registered nurse is $25.16/hr, but this extends to a ceiling of $55.86/hr. The median hourly earnings in Australian nursing in 2019 was $36/hr. Many of today’s nurses are highly innovative and engaged, and increasingly efficient as a result.
So, while nurses may cost more to employ now than 50 years ago, they also contribute much more. The aged-care sector can certainly learn from this.
The benefits of professionalisation
Regardless of the royal commission’s specific findings, the Australian government will inevitably need to provide a more robust funding model to the aged-care sector to help meet the complex health needs of older Australians.
Yet research conducted as part of the royal commission has highlighted cost inefficiencies in the current system. We argue these inefficiencies can be mitigated by further professionalising the aged-care workforce.
Valuing the aged-care workforce as a profession will require investment in training. Improving access to higher levels of training for all aged-care workers will deliver a range of benefits: the workforce will become more adaptable, agile and innovative. This will prepare them for integration with new technologies such as Robear, the nursing-care robot.
Read more: Nurses of the future must embrace high-tech
If the COVID pandemic has taught us anything, it’s that governments can, when there is strong public appetite, spend significantly to resolve major crises. If left on its current trajectory, the aged-care sector may implode – particularly if we lose access to migrant labour as a result of our closed international borders.
It’s time to work smarter, not harder, and invest in the future of our aged-care workforce. There is every chance most Australians alive today will reap the benefits of a more engaged, innovative and productive aged-care workforce.
Authors: Ben Farr-Wharton, Associate Dean of Management, Edith Cowan University





