when is a colonoscopy necessary?
- Written by Suzanne Mahady, Gastroenterologist & Clinical Epidemiologist, Senior Lecturer, Monash University
From time to time, we hear or read about medical procedures that can be ineffective and needlessly drive up the nation’s healthcare costs. This occasional series will explore such procedures individually and explain why they could cause more harm than good in particular circumstances.
A recent study found around 30% of all procedures performed in a New South Wales hospital were either unhelpful or harmful. Some of these, which included performing a colonoscopy for constipation, were becoming more prevalent.
A colonoscopy is a test where a small, flexible tube is inserted into the bowel to check for abnormalities such as growths on the bowel, which can lead to bowel cancer.
Around 600,000 colonoscopies were performed in Australia in 2013-2014. This figure is expected to rise to more than a million a year by 2020, equivalent to one in every 25 Australians.
A colonoscopy is an invasive procedure and comes with risks, including bowel perforation. So, it’s important to have the test only if you’re likely to benefit from it.
Why are colonoscopies performed?
Bowel cancer is the second-most-common cause of cancer-related death in Australia. Current evidence suggests colonoscopy significantly reduces the risk of bowel cancers. This is where colonoscopy’s greatest benefit lies. Colonoscopy can also be used to diagnose inflammatory bowel diseases.
Read more: Explainer: what is inflammatory bowel disease?
Bowel cancers start out as small growths in the bowel called polyps. These can be seen with a colonoscopy and cut out by doctors during the test.
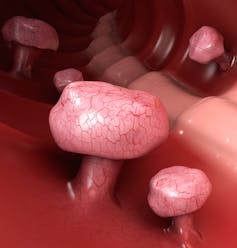 A colonoscopy can check for polyps, which are small growths on the bowel.
from shutterstock.com
A colonoscopy can check for polyps, which are small growths on the bowel.
from shutterstock.com
So, colonoscopy is more worthwhile when done in people at an increased risk of bowel cancer. The most important risk factor is age, as cancer rates increase in people older than 50.
But some younger people can be at risk due to family history. And recent data suggest bowel cancer in young people is rising here and internationally, though we’re not sure why.
Who should have a colonoscopy?
A doctor will usually recommend a colonoscopy if patients are at increased risk of bowel cancer due to family history (particularly first-degree relatives who develop bowel cancer before the age of 55), if their “poo test” is positive for blood, or if they have concerning symptoms such as bleeding.
Read more: Pre-cancerous: warning sign or cause for panic?
An Australian study tried to determine which symptoms could best predict bowel cancer. The authors collected data on around 8,000 patients with a range of symptoms – including rectal bleeding and constipation – undergoing colonoscopy. They followed them to see who was diagnosed with a cancer (or a large polyp) during the colonoscopy.
They found that, apart from age, rectal bleeding was the strongest predictor of bowel cancer. Other common symptoms such as abdominal pain or constipation alone were not associated with bowel cancer, suggesting colonoscopy in these cases was unnecessary. These findings have been replicated in other studies.
When not to have a colonoscopy
Small polyps grow slowly and may take ten years or longer (if at all) to develop into bowel cancer. This is why it is considered inappropriate to continue screening in people aged over 75.
International speciality groups don’t recommend ongoing screening when life expectancy is less than ten years, because many people will not benefit. And they will be exposed to the risks of colonoscopy, including bowel perforation and major bleeding. Australian guidelines also recommend stopping colonoscopy in people aged around 75.
Read more: Costly and harmful: we need to tame the tsunami of too much medicine
In young people, colonoscopy is often performed to look for inflammatory bowel disease, but new non-invasive stool tests can select out people at higher risk. Young people with irritable bowel syndrome may also undergo repeated colonoscopies to try to find an alternative reason for their symptoms, but this strategy is usually unhelpful.
Why are colonoscopies on the rise?
Australia’s population is ageing and the number of people older than 55 is increasing.
Consumer demand can also drive unnecessary testing. Evidence shows that people frequently overestimate the benefits and underestimate the harms of tests such as colonoscopy. Often there’s a misconception that more tests and more health care leads to better health, when data suggest the opposite is true.
The global Choosing Wisely campaign aims to educate consumers about risks of over-testing. In the future, symptoms-based algorithms and new diagnostic tests might improve a doctor’s ability to identify those at increased risk of bowel cancer for colonoscopy.
In the meantime, prioritising colonoscopy for patients who are at higher risk should be the goal.
Authors: Suzanne Mahady, Gastroenterologist & Clinical Epidemiologist, Senior Lecturer, Monash University
Read more http://theconversation.com/needless-medical-procedures-when-is-a-colonoscopy-necessary-102576





