Hospitals are risky places – but some are better than others
- Written by Stephen Duckett, Director, Health Program, Grattan Institute
One in every nine patients who go into hospital in Australia suffers a complication: when something preventable goes wrong with their care. They might develop an infection from a hygiene breach, for instance, or be given the wrong dose or type of drug.
Or the complication might be less direct, such as becoming malnourished because you haven’t been monitored well enough, or developing a pressure sore because you’ve spent too long in the same position in your hospital bed.
A new Grattan Institute report, All complications should count: Using our data to make hospitals safer, reveals the risk of a complication varies markedly between hospitals. It argues that patients need to know about these risks, and hospitals need to have this information to help them reduce risks for patients.
Read more: Why you should avoid hospitals in January
Australian hospitals collect a lot of information about the patients they treat. This information is used to work out how much each hospital is paid for the work they do. But it should also be a powerful tool for improving safety of care.
Rate of complications
Our report shows that the rate of complications for people admitted for a same-day treatment is very low, around 3%. But an astounding one in four patients who have an overnight stay endures a complication.
The rate of complications varies markedly between hospitals. We have data on every complication and every hospital, although the hospitals are de-identified. The potential value of this data is illustrated by the graph below, which looks at just one procedure – knee replacements – at three hospitals.
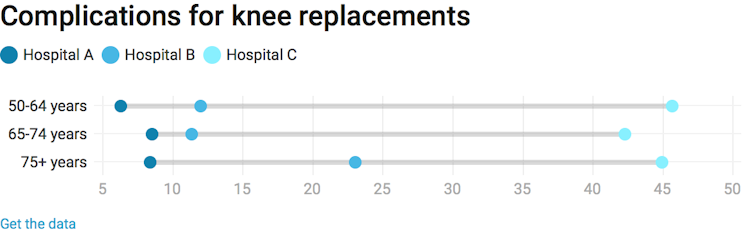 It shows Hospital A is a uniformly good hospital to go to for a knee replacement, and Hospital C is uniformly bad. At Hospital B, patients over 75 face twice the excess risk of a complication than patients between the ages of 50 and 74.
This isn’t all simply luck of the draw. Hospital A is obviously doing things better. Hospitals B and C may be lacking specialist geriatric support for elderly patients. The other hospitals should learn from Hospital A about how to lift their game.
Yet most Australian hospitals don’t receive this sort of detailed comparative information, so they cannot compare themselves to their peers and learn from the better performers.
Information needs to be shared
These huge variations in complication rates are important. More complications means more pain and discomfort for patients. Higher complication rates mean longer hospital stays, which in turn mean higher costs for the health system. Higher complication rates contribute to higher health insurance premiums, too.
Patients should have information about their chances of complications. They should know what their risk is, taking into account their age, gender and general state of health. They should also know what types of risks they face, from the rare but catastrophic to the less dramatic but more prevalent.
Read more:
Infections, complications and safety breaches: why patients need better data on how hospitals compare
State governments and private health insurers have this information now. They should share it. They should publish information on complication rates at different hospitals, so that patients – and their referring general practitioners – can know what difference it makes, in terms of complications, going to one hospital compared to another.
This vital comparative complication rate information is generally not even provided to hospitals themselves. Although some states and some private health insurers have feedback programs – where they provide information adjusted for the mix of patients treated in the hospital – such programs are not universal, they are not comprehensive, and the data is often old.
This means hospitals are flying blind when designing safety improvement efforts. They don’t know how they are performing against their peers. They don’t know whether they are the best in class or the worst. They don’t know where they need to improve, or by how much they should improve. They don’t know how they measure up in terms of infection rates among their patients, or falls, or complications arising from procedures.
It shows Hospital A is a uniformly good hospital to go to for a knee replacement, and Hospital C is uniformly bad. At Hospital B, patients over 75 face twice the excess risk of a complication than patients between the ages of 50 and 74.
This isn’t all simply luck of the draw. Hospital A is obviously doing things better. Hospitals B and C may be lacking specialist geriatric support for elderly patients. The other hospitals should learn from Hospital A about how to lift their game.
Yet most Australian hospitals don’t receive this sort of detailed comparative information, so they cannot compare themselves to their peers and learn from the better performers.
Information needs to be shared
These huge variations in complication rates are important. More complications means more pain and discomfort for patients. Higher complication rates mean longer hospital stays, which in turn mean higher costs for the health system. Higher complication rates contribute to higher health insurance premiums, too.
Patients should have information about their chances of complications. They should know what their risk is, taking into account their age, gender and general state of health. They should also know what types of risks they face, from the rare but catastrophic to the less dramatic but more prevalent.
Read more:
Infections, complications and safety breaches: why patients need better data on how hospitals compare
State governments and private health insurers have this information now. They should share it. They should publish information on complication rates at different hospitals, so that patients – and their referring general practitioners – can know what difference it makes, in terms of complications, going to one hospital compared to another.
This vital comparative complication rate information is generally not even provided to hospitals themselves. Although some states and some private health insurers have feedback programs – where they provide information adjusted for the mix of patients treated in the hospital – such programs are not universal, they are not comprehensive, and the data is often old.
This means hospitals are flying blind when designing safety improvement efforts. They don’t know how they are performing against their peers. They don’t know whether they are the best in class or the worst. They don’t know where they need to improve, or by how much they should improve. They don’t know how they measure up in terms of infection rates among their patients, or falls, or complications arising from procedures.
 Greater transparency about complications can lead to safety improvements.
Piron Guillaume
Worse, current government priorities encourage hospitals to focus on a subset of complications which only affect a fraction of patients and aren’t relevant to all specialties. This may lull hospitals into a false sense of security that they have no room to improve when in fact their overall performance – looking at all complications – may be very poor indeed.
How to reduce complications
Until all hospitals have all relevant information on their comparative complication rates, identifying where to start their improvement efforts is impossible. Our report recommends four simple solutions:
all states and territories establish goals for reducing the overall rate of complications in public and private hospitals
all states and territories give hospitals and clinicians the ability to interrogate the state hospitals data (without individual patients being able to be identified), so they can see how their performance measures up against the best-performing hospitals and clinicians. All hospitals develop strategies to identify opportunities to improve
all states and territories publish reports on excess complications, by specialty and institution (including private hospitals)
major private health insurers provide their members with comparative information on complication rates.
All these proposals could be implemented tomorrow. For the sake of Australian taxpayers and hospital patients, they should be.
Greater transparency about complications can lead to safety improvements.
Piron Guillaume
Worse, current government priorities encourage hospitals to focus on a subset of complications which only affect a fraction of patients and aren’t relevant to all specialties. This may lull hospitals into a false sense of security that they have no room to improve when in fact their overall performance – looking at all complications – may be very poor indeed.
How to reduce complications
Until all hospitals have all relevant information on their comparative complication rates, identifying where to start their improvement efforts is impossible. Our report recommends four simple solutions:
all states and territories establish goals for reducing the overall rate of complications in public and private hospitals
all states and territories give hospitals and clinicians the ability to interrogate the state hospitals data (without individual patients being able to be identified), so they can see how their performance measures up against the best-performing hospitals and clinicians. All hospitals develop strategies to identify opportunities to improve
all states and territories publish reports on excess complications, by specialty and institution (including private hospitals)
major private health insurers provide their members with comparative information on complication rates.
All these proposals could be implemented tomorrow. For the sake of Australian taxpayers and hospital patients, they should be.
Authors: Stephen Duckett, Director, Health Program, Grattan Institute
Read more http://theconversation.com/hospitals-are-risky-places-but-some-are-better-than-others-91057





